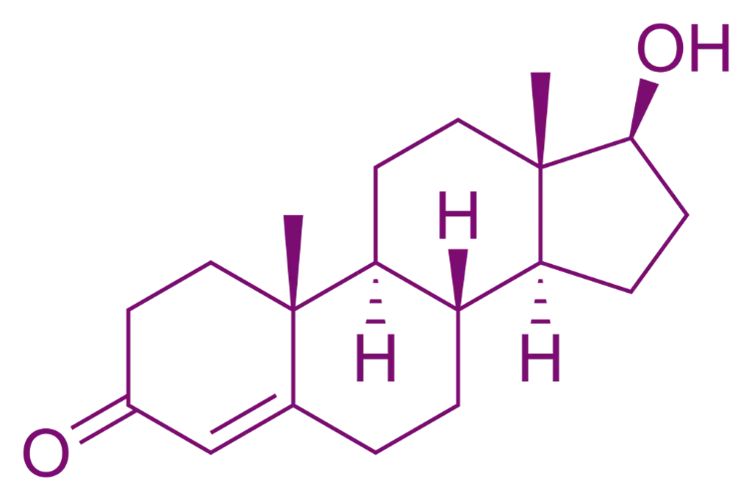
Definition of Androgens:
- Androgens are male sex hormones responsible for developing and maintaining male characteristics. The primary endogenous androgen is testosterone.
Physiological Roles:
- Produced mainly by Leydig cells in the testes and, to a lesser extent, by the adrenal cortex.
- Regulate development of male secondary sexual characteristics, spermatogenesis, and libido.
- Exhibit anabolic effects: Promote protein synthesis, increase muscle mass, and stimulate erythropoiesis.
Physiology of Androgens:
- Major Androgens: Testosterone, Dihydrotestosterone (DHT, more potent), and Androstenedione.
- Regulation: Controlled by the hypothalamic-pituitary-gonadal (HPG) axis:
- Hypothalamus releases GnRH → Stimulates anterior pituitary to release LH → LH stimulates Leydig cells to produce testosterone.
Pharmacological Actions:
-
Androgenic Actions:
- Development and maintenance of male secondary sexual characteristics (facial hair, deep voice, etc.).
- Growth of male reproductive organs.
-
Mechanism of Action:
- Androgens bind to androgen receptors in target tissues, regulating gene expression and promoting male characteristics.
Pharmacological Agents:
- Testosterone: Natural androgen used for hypogonadism, delayed puberty, and breast cancer.
- Synthetic Androgen: Methyltestosterone, Fluoxymesterone—enhance androgenic effects and improve pharmacokinetics.
Clinical Uses of Androgens:
- Hypogonadism: Replacement therapy to restore testosterone levels.
- Delayed Puberty: Induction of puberty in adolescent males.
- Anemia: Stimulates erythropoiesis.
- Breast Cancer: Inhibits estrogen-dependent tumor growth.
Side Effects:
- Androgenic Effects: Acne, hair loss (male pattern baldness), and increased body hair.
- Estrogenic Effects: Gynecomastia due to aromatization of testosterone to estradiol.
- Other Risks: Liver toxicity (especially with oral forms), cardiovascular risks, mood swings, and infertility due to suppression of the HPG axis.
Click Here to Watch the Best Pharma Videos