ANTI-ARRHYTHMIC DRUGS
- BP-S-5-MEDICINAL CHEMISTRY
- Dec 21, 2024
- 2 min read
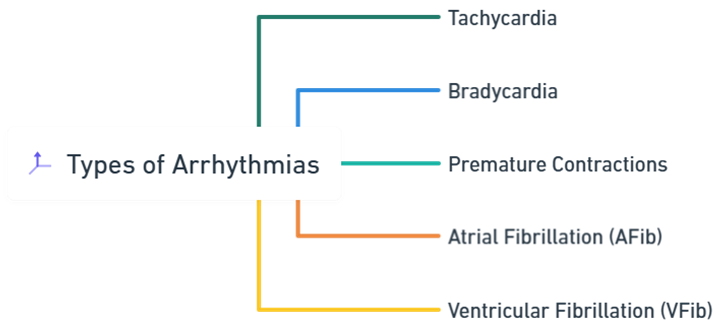
Anti-arrhythmic drugs are medications used to treat and prevent abnormal heart rhythms (arrhythmias).
These drugs work by modifying the electrical activity of the heart to restore and maintain a normal heart rhythm, thereby ensuring efficient blood circulation throughout the body.
Pathophysiology of Arrhythmias
Arrhythmias occur due to disturbances in the normal electrical conduction system of the heart. These disturbances can result from:
Enhanced Automaticity: Increased spontaneous depolarization of cardiac cells.
Triggered Activity: Abnormal depolarizations during or after repolarization.
Reentrant Circuits: Circular electrical pathways that perpetuate abnormal rhythms.
Anti-arrhythmic drugs aim to correct these disturbances by targeting various aspects of cardiac electrophysiology.
Classification of Anti-Arrhythmic Drugs
Anti-arrhythmic drugs are primarily classified according to the Vaughan Williams Classification, which categorizes these medications based on their primary mechanism of action on cardiac cells.

1) Class I: Sodium Channel Blockers
These drugs inhibit sodium (Na⁺) channels, reducing the rate of rise of the action potential (phase 0) in cardiac cells. They are further subdivided into:
A) Class IA
Mechanism: Moderate blockade of Na⁺ channels; also block potassium (K⁺) channels, prolonging action potential duration and refractory period.
Drugs:
Quinidine Sulphate
Procainamide Hydrochloride
Disopyramide Phosphate
Uses: Atrial and ventricular arrhythmias.
Side Effects: Prolonged QT interval, torsades de pointes, hypotension.
B) Class IB
Mechanism: Mild blockade of Na⁺ channels; shorten action potential duration and refractory period.
Drugs:
Lidocaine Hydrochloride
Phenytoin Sodium
Tocainide Hydrochloride
Uses: Ventricular arrhythmias, especially post-myocardial infarction.
Side Effects: CNS toxicity (e.g., seizures, tremors), numbness.
C) Class IC
Mechanism: Potent blockade of Na⁺ channels with minimal effect on action potential duration.
Drugs:
Mexiletine Hydrochloride
Lorcainide Hydrochloride
Uses: Atrial and ventricular arrhythmias.
Side Effects: Bradycardia, hypotension, proarrhythmic effects.
2) Class II: Beta Blockers
These drugs block beta-adrenergic receptors, decreasing the effects of sympathetic stimulation on the heart.
Mechanism: Reduce heart rate, myocardial contractility, and conduction velocity through the atrioventricular (AV) node.
Drugs:
Sotalol
Uses: Atrial fibrillation, ventricular arrhythmias, prevention of arrhythmic recurrence.
Side Effects: Bradycardia, hypotension, fatigue, bronchoconstriction.
3) Class III: Potassium Channel Blockers
These drugs primarily block K⁺ channels, leading to prolonged repolarization and extended action potential duration.
Mechanism: Prolong the QT interval and the refractory period without affecting Na⁺ or Ca²⁺ channels significantly.
Drugs:
Amiodarone
Uses: Atrial fibrillation, ventricular tachycardia, ventricular fibrillation.
Side Effects: Pulmonary fibrosis, thyroid dysfunction, liver toxicity, corneal deposits.
Class | Mechanism | Drugs | Uses | Side Effects |
Class I: Sodium Channel Blockers (IA) | Moderate Na⁺ & K⁺ blockade; prolongs action potential and refractory period | Quinidine, Procainamide, Disopyramide | Atrial and ventricular arrhythmias | Prolonged QT interval, torsades de pointes, hypotension |
Class I: Sodium Channel Blockers (IB) | Mild Na⁺ blockade; shortens action potential duration and refractory period | Lidocaine, Phenytoin, Tocainide | Ventricular arrhythmias, especially post-MI | CNS toxicity (seizures, tremors), numbness |
Class I: Sodium Channel Blockers (IC) | Potent Na⁺ blockade; minimal effect on action potential duration | Mexiletine, Lorcainide | Atrial and ventricular arrhythmias | Bradycardia, hypotension, proarrhythmic effects |
Class II: Beta Blockers | Beta-adrenergic receptor blockade; reduces heart rate and AV node conduction | Sotalol | Atrial fibrillation, ventricular arrhythmias | Bradycardia, hypotension, fatigue, bronchoconstriction |
Class III: Potassium Channel Blockers | K⁺ channel blockade; prolongs QT interval and refractory period | Amiodarone | Atrial fibrillation, ventricular tachycardia, ventricular fibrillation | Pulmonary fibrosis, thyroid dysfunction, liver toxicity, corneal deposits |








留言